AHL Newsletter June 2019
Click here for a pdf copy of the June 2019 AHL Newsletter.
Dr. Maxie retires, May 31, 2019
After 22 years as AHL Director, including 12 years as co-Executive Director of Laboratory Services Division, Grant Maxie is retiring.
Beginning in Guelph as an intern in OVC right after graduation from the Western College of Veterinary Medicine in Saskatoon in 1969, Grant has been in and about Guelph for the past 50 years. After his internship, he completed his PhD in clinical pathology under the guidance of Dr. Ted Valli. He then undertook a 3-year stint as a hematologist within the International Development Research Center project in Kenya on trypanosomiasis (sleeping sickness of cattle) and theileriosis (East coast fever).
Returning to OVC as faculty in the Department of Pathology, he taught cardiovascular and urinary pathology for 5 years before moving to the Veterinary Services Branch of OMAFRA in 1982 as an anatomic pathologist, completing the ACVP boards in 1984, and becoming Guelph lab head in 1994. VLSB was transferred to the U of Guelph in 1997 as part of the Common Sense Revolution; Lab Services is administered within the Office of Research.
Retirement plans include continuing as editor-in-chief of the Journal of Veterinary Diagnostic Investigation, farming (hay-making, fence building), home repairs, travel, spending time with family, dancing, and the occasional round of golf. AHL
May 1, 2019, AHL User’s Guide and Fee Schedule
- Includes more test information, new tests, new test panels, fee adjustments, and more!
- Mobile friendly!
- Available on-line at https://www.uoguelph.ca/ahl/
- Test information is linked to LabNotes to facilitate test selection and interpretation of results.
Update on histopathology and postmortem tests at the AHL:
| Histopathology | Test code |
| - on food animal PM or mail-in | pmfd |
| - on companion/other, 1-2 biopsies or tissues, equine abortion | histcm1 |
| - on companion/other, 3-6 biopsies or tissues | histcm2 |
| - on companion/other, 7 or more biopsies or tissues, including AHL PMs | histcm3 |
Additional fees may be applied for pathologists to sample large or complex specimens, IHC, tumor margins, >10 slides, and special stains. For immunohistochemistry (IHC) cases originating from external laboratories, please note that transportation (courier) fees will be charged for slide and block return to the submitting laboratory.
| Postmortem | Test code |
| Postmortem, companion/other | pmca |
| Postmortem, companion/other, pocket-sized | pmpp |
| Postmortem, equine abortion, stillbirth, or <24 h neonate | pmea |
Please check the AHL Fee Schedule booklet or visit our website for full testing details https://www.uoguelph.ca/ahl/tests.
Client access is required.
For species categories, refer to the AHL website – Case definition for billing purposes - https://www.uoguelph.ca/ahl/billing-and-fees
Premises ID and Client Portal
Jim Fairles, Josie Given
In partnership with OMAFRA, the Animal Health Laboratory will assist veterinary clinics and their clients in obtaining their premises ID (PID). A single agreement with AHL is signed by the clinic stating that any premises information provided to the laboratory was done with the client’s consent.
Together, we can work to quickly and efficiently get the PID numbers added to your client database. Once the client has been assigned a PID, a PPR certificate will be either emailed (preferred) or sent by mail to the owner of the premises.
AHL also now has a Client Portal for online submissions. Once your client PIDs are obtained, using the portal will:
- Standardize your lab submissions (spelling of owner names, PID, farm name, etc.).
- Track the progress of your cases, edit/cancel before the specimen is received at AHL.
- Allow advanced searching, design reports based on Animal ID, farm, owner, etc.
- Provide a case # prior to sending to AHL & track its progress as results are released.

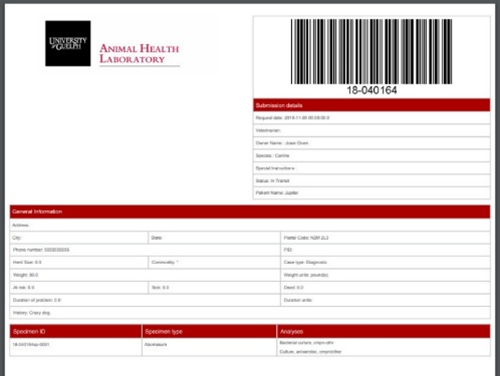
Contact Josie Given: 519-824-4120 ext 54320, or jgiven@uoguelph.ca to setup training! AHL
Ontario Animal Health Network
OAHN Update - June 2019
OAHN wishes to acknowledge the extensive contributions of AHL Director Dr. Grant Maxie to the network. As program director for OAHN since its inception in 2013, Dr. Maxie was instrumental in establishing the networks, “steering the ship” along the way, and guiding OAHN to its current stable and productive state. He provided a wealth of knowledge and experience, and was incredibly supportive of all of the new ways we approached communication of animal health news to our members and followers. We wish him the best in his retirement, and hope he keeps up with the new and exciting projects we have planned for the future.
New Infographics


The OAHN Companion Animal Network has recently released new infographics about Feline Upper Respiratory Tract Disease and Antibiotics, Laboratory Submissions, Itchy Dogs: Topical Treatments and Culture-Critical Cases. Additionally, the network has updated its Echinococcus multilocularis infographic to reflect the most up-to-date data and figures about EM in Ontario.
The OAHN Equine Network has created an in-depth infographic looking at equine herpes myeloencephalopathy. The infographic covers prevention, risk of disease, clinical signs, diagnosis, treatment, and reducing the spread of EHM. There was a confirmed case of EHM in the Regional Municipality of York in April.
OAHN Small Flock Poultry Veterinary Seminar
On April 6, the OAHN Poultry Network organized and hosted a Small Flock Veterinary workshop at the Animal Health Laboratory . The day consisted of expert presentations on small flock health and management, followed by wet labs in the PM room, where vets were given the opportunity for some more applied work. The day was a huge success, with 40 veterinarians from around Ontario attending, with Dr. Victoria Bowes, board-certified poultry veterinarian and diagnostic avian pathologist, as keynote speaker. Thanks to everyone from the OAHN Poultry Network for making this day a success, and thanks to all of the vets for attending.
New Reports
The Q1 2019 network reports for most networks have been posted to the OAHN site—just select the species you wish to view under “Network Reports”. Some highlights include:
- Companion Animals: Vets are seeing less respiratory disease and more multi-drug resistant bacterial infections; “New” canine distemper strains; encephalitis from raccoon roundworm; rabies update.
- Swine: Keeping ASF and other diseases out of your barn; OAHN Swine erysipelas project update; more PEDV and PDCoV on farms in Ontario.
- Bovine: Ureaplasma abortions in 2019; veterinary surveillance; OAHN research project; case report on malignant catarrhal fever.
- Poultry: Veterinary survey highlights; antimicrobial prescription changes.
We have lots of new reports, lab data, and resources. Be sure to check out OAHN.ca
RUMINANTS
Abortion caused by Helicobacter trogontum in a sheep flock
Maria Spinato, Margaret Stalker, Durda Slavic, John McNally
A producer with a flock of 250 Bluefaced Leicester and Scottish Blackface sheep reported 3 abortions of near-term fetuses in a group of 52 breeding ewes. This group of crossbred ewes had been recently purchased and relocated from Saskatchewan. Two additional abortions had occurred previously; however, fetuses were at an earlier stage of gestation, and diagnostic testing was not pursued. Ewes appeared to be healthy, in good body condition, and had been recently vaccinated and dewormed. The ration consisted of corn silage, oats, and free-choice hay. Samples of fresh placenta obtained from two abortions were submitted to the AHL for testing.
Cotyledons in one placenta were noted to be mildly swollen. Samples of placenta were submitted for culture for common bacterial pathogens including Campylobacter spp., PCR testing for Coxiella and Chlamydia, and histologic examination. No significant bacterial pathogens were isolated in culture, and PCR tests for Coxiella and Chlamydia were negative. Histologic features in both placentas were similar: autolysis was moderately advanced and trophoblastic epithelium was sloughed. Extensive infiltrates of neutrophils were present within both cotyledonary and intercotyledonary chorioallantois (Fig. 1). In one placenta, several allantoic arterioles were undergoing leukocytoclastic vasculitis, associated with occasional thrombosis. Based upon the histologic findings of marked suppurative placentitis, further testing for infectious causes of ovine abortion was initiated. PCR testing for Toxoplasma and Leptospira was negative, and immunohistochemical staining for BVDV/Border disease virus was also negative.
Reports in the literature of sporadic cases of ovine abortion caused by Flexispira rappini in New Zealand and the United States caused us to pursue further PCR testing of saved frozen portions of placenta using genus-specific Helicobacter primers. The obtained PCR product was sequenced, and sequence results (100% coverage and 99.4% identity) revealed the presence of Helicobacter trogontum, previously known as Helicobacter (Flexispira) rappini. Additionally, immunohistochemical staining of the placental lesions using rabbit anti-H. pylori polyclonal antibodies (Dako) revealed widespread positive immunostaining (note: previous literature reports have described cross-reactivity of this antiserum with multiple Helicobacter species) (Fig. 2).
A recent retrospective diagnostic survey of laboratory submissions from ovine abortion outbreaks in New Zealand (NZ) identified Helicobacter bilis and Helicobacter trogontum as causes of late-term abortions in a small, but significant proportion of affected flocks. In the NZ outbreaks, postmortem and histologic lesions in affected fetal livers resembled those of Campylobacter spp., consisting of hepatomegaly and multifocal hepatic necrosis. Large curved bacilli situated within viable hepatocytes bordering necrotic foci were visualized by positive Warthin-Starry silver staining. The authors described one case that was positive for Helicobacter spp. by PCR and that lacked hepatic lesions. Placentas were not available for examination.
This is the first identification by the AHL of Helicobacter trogontum as a cause of placentitis and abortion in sheep. Whether this organism is a sporadic, previously undetected or emerging cause of infectious ovine abortion in Ontario remains to be elucidated. Much remains unknown regarding the source of the organism, the method of transmission and its pathogenicity. Molecular tools have now provided us with the means of answering some of these questions. AHL
Reference
Gill J, et al. Helicobacter bilis and Helicobacter trogontum: infectious causes of abortion in sheep. J Vet Diagn Invest 2016;28:225-234.

Figure 1. Autolysed chorioallantois infiltrated by neutrophils.

Figure 2. Positive IHC staining for Helicobacter spp. in ovine placenta.
Complex vertebral malformation syndrome in a full-term Holstein fetus
Heindrich Snyman, Henry Ceelen
A single full-term, fully haired, aborted Holstein fetus, and its associated placenta and attached umbilical cord was received by the AHL-Kemptville for postmortem evaluation. The fetus originated from a heifer that had reached her due date but had failed to show any premonitory signs of calving. The dam was subsequently induced (10 mL dexamethasone, 3 mL cloprostenol) but failed to progress and the dead fetus was ultimately delivered via caesarian section.
At postmortem there was marked shortening of the neck, and the cervical profile was irregular (Fig. 1). The cranial-to-caudal thoracic vertebral column was similarly irregular and had moderate scoliosis. All 4 limbs were fixed with arthrogryposis (Fig. 1). The head was smaller than expected with subtle rostro-caudal shortening, doming, and incomplete coverage of the caudal cranial sutures forming and ~ 2.0 x 1.6 cm retained inter-sutural space. There was no herniation or extension of meninges or brain from this site. Upon opening the calvaria, the brain was very soft and collapsed on removal (suspect hydrocephalus). The vertebral column was split mid-sagittally to evaluate the vertebral bodies. Within the cervical vertebral column, vertebral bodies C3 to C7 were irregular, small and angular-to-wedge-shaped and there was partial fusion of the C5/C6 vertebrae (Fig. 2). Similar shortening and irregularity was observed within the T1 to T5 thoracic vertebrae, but changes were less obvious than for the cervical vertebrae. The ribs and sternum as well as the lumbar and sacral vertebrae appeared grossly unremarkable. The heart was globose and flaccid with biventricular dilation and a 1.2-cm ventricular septal defect ~1 cm below the aortic semilunar valves (Fig. 3). The lungs were not inflated and there was mild associated pulmonary congestion and edema. The changes noted in the cervical and thoracic vertebral column, head, and heart are characteristic of complex vertebral malformation (CVM). In addition, both the dam and sire were known carriers for CVM. With the assistance of Holstein Canada, samples of fetal skeletal muscle was sent for genetic testing and the fetus was found to be “CVM affected”.
CVM is a congenital autosomal recessively inherited disorder of Holstein cattle resulting from a single base missense substitution in the nucleotide sugar transporter gene SLC35A3. It has been traced back to the US Holstein sire Penstate Ivanhoe Star and one of his sons Carlin-M Ivanhoe Bell and their offspring, and represents the single most prevalent inherited disorder in Holstein cattle. CVM-affected fetuses are aborted ~75% of the time with the remaining ~25% usually terminating in stillbirths. The SLC35A3 transporter plays a significant role in NOTCH signalling and the formation of the vertebral column during embryonic development and differentiation of the unsegmented paraxial mesoderm. As a result, this syndrome is associated with significant cervical and thoracic vertebral malformation, malformed ribs, and arthrogryposis. Additionally, cardiac anomalies are also often reported (including septal defects, great vessel malformation, and myocardial hypertrophy). AHL
References
Agerholm JS, et al. Complex vertebral malformation in Holstein calves. J Vet Diagn Invest 2001;13:283-289.
Thomsen B, et al. A missense mutation in the bovine SLC35A3 gene, encoding a UDP-N-acetylglucosamine transporter, causes complex vertebral malformation. Genome Res 2006;16:97-105.

Figure 1. Aborted Holstein fetus with irregular and shortened neck and arthrogryposis.

Figure 2. Mid-sagittal split vertebral column with irregular wedge-shaped C3-C7 cervical vertebral bodies (arrows) and partial fusion of the C5/C6 vertebrae (asterisk).

Figure 3. Heart with high ventricular septal defect (arrow).
FISH
Concurrent bacterial gill disease and nodular gill disease in rainbow trout fingerlings
Heindrich Snyman, Nikki LePage, Kathleen Todd, Calvin Kellendonk, Patricia Bell-Rogers, Lisa Ledger, Qiumei You, Hugh Cai
During late February, a commercial aquaculture hatchery was experiencing increased daily mortality rates in a group of ~ 25 g, triploid, rainbow trout (Oncorhynchus mykiss) fingerlings. Fish were routinely raised in indoor fiberglass pens prior to being moved to outside concrete raceways in December of the preceding year. Throughout the initial growing period, mortality rates were stable until a low but steady increase was observed starting ~1 wk prior to submission.
Live fish (n = 18) were submitted to the AHL for testing. Fish had open mouths with flared opercula, patchy pale gills, and overlying tacky mucus on the gill surfaces. Some fish had eroded fins with skin ulcers overlying the operculum and lateral abdominal surfaces. Wet mounts of gill clips revealed large dense mats of slender filamentous bacteria with occasional scattered diatoms (Fig. 1). Histologically, widespread lamellar epithelial hyperplasia often spanned the entire length of individual filaments and resulted in extensive lamellar fusion and formation of interlamellar pockets with entrapped sloughed cellular debris (Figs. 2, 3). Interfilamentous spaces, remaining interlamellar spaces, and pockets, contained, dense colonies of ~0.5 µm wide and 2.0-5.0 µm long slender filamentous bacteria (Fig. 2) with abundant ~8-15 µm, irregular angular-to-polygonal, non-ciliated protozoa, with small eccentric magenta nuclei and fine granular basophilic cytoplasm (amoebic trophozoites) (Figs. 3, 4). These changes were consistent with a diagnosis of both bacterial gill disease (BGD) and nodular gill disease (NGD).
BGD is one of the most significant infectious diseases affecting freshwater salmonid aquaculture worldwide. The causative agent is Flavobacterium branchiophilum, a gram-negative, non-motile, slender filamentous bacterium. Disease outbreaks are especially common in intensively reared fry and fingerlings and often occur during early spring and summer when higher temperatures and rising precipitation are implicated as causative factors. Aerobic culture of gill surface swabs in our case however yielded a Flavobacterium sp. different from F. branchiophilum, confirmed by MALDI-TOF MS. The full sequence of the 16S rRNA gene of the isolate had 98.8% identity to an unidentified Flavobacterium sp. WB 4.2-31 (1460/1478 bp), and 98.7% similarity to a F. aquidurense (1459/1478 bp). Although other flavobacterial pathogens can cause similar or concurrent gill lesions, this has been historically uncommon in Ontario. Nonetheless, in recent years a small number of unidentified Flavobacterium spp., similar to our case, have been isolated in AHL submissions seen as bacterial gill disease. This suggests that strains other than F. branchiophilum could also contribute to the development of clinical bacterial gill disease.
NGD represents the second most common gill disease affecting Ontario rainbow trout aquaculture. Cochliopodium sp. is the most common cause in Ontario, although other pathogenic gill amoebas also exist in other production systems and fish species (e.g., Paramoeba sp., Thecamoeba sp., etc.). NGD follows a clinical presentation similar to BGD, although mortality and morbidity rates are typically lower. Concurrent infection with filamentous bacteria is not unusual as amoebas are particularly attracted to surface filamentous bacteria and cell debris, which act as a rich nutrient source for amoeba.
Co-infected cases will respond poorly to standard BGD antibacterial treatments (e.g., chloramine-T) and given the similarities in clinical presentation, appropriate laboratory testing (including gill wet mounts and histopathology) is a necessity to ensure an accurate diagnosis. AHL
References
Ferguson H, et al. Systemic Pathology of Fish. Scotian Press..2nd ed. 2006. ISBN-10: 0955303702.
Ferguson H, et al. Gill diseases of fish in Ontario farms. OMAFRA fact sheet. 1994. ISBN 0-7778-2306-3.
Noga E. Fish Disease: Diagnosis and Treatment. Wiley-Blackwell; 2nd ed. 2010. ISBN-10: 0813806976.

Figure 1. Gill clip wet mount with mats of slender filamentous bacteria (asterisks).

Figure 2. Histology of gills with widespread lamellar epithelial hyperplasia with fusion (arrow) and dense filamentous bacteria (asterisks).

Figure 3. Histology of gills with widespread lamellar epithelial hyperplasia, fusion, and pocket formation (arrow) with interspersed amoebic trophozoites (asterisks).

Figure 4. Histology of gills with amoebic trophozoites (arrows).
SWINE
African swine fever – resources for veterinarians
African Swine Fever (ASF) is a very real disease threat that could potentially infect North American swine of all types, including small specialty herds and companion swine. All veterinarians, including companion and mixed animal practitioners, should familiarize themselves with the clinical signs, gross lesions, and routes of transmission of ASF.
The Canadian Pork Council has produced numerous information pieces regarding ASF and risk mitigation practices including for small scale producers. These are available on their website at https://www.cpc-ccp.com/ASF-resources-printables .
In December, the Canadian Animal Health Surveillance System (CAHSS) and the Community for Emerging and Zoonotic Diseases (CEZD) hosted French and English webinars on ASF, which are available as taped versions:
https://gts-ee.webex.com/gts-ee/ldr.php?RCID=52a493fdfed537869eafe8d166b131ad (Disregard the ‘no content’ note once the presentation loads do – just start the recording.)
Additional images of ASF gross lesions of African Swine Fewer have been published online by the Center for Food Security and Public Health, Iowa State University:
http://www.cfsph.iastate.edu/DiseaseInfo/disease-images.php?name=african-swine-fever&lang=en
Chlamydia suis and Mycoplasma suis PCRs now available at the AHL
Hugh Cai, Josepha DeLay
Chlamydia suis and C. abortus are the main species involved in chlamydial infections in pigs. C. suis can cause conjunctivitis, pneumonia, enteritis, and reproductive failure, which has been reported in Belgium, Cyprus, Estonia, Germany, Israel, Switzerland, and China. Concern has been raised in Ontario and in other swine-producing areas of North America about possible contribution of C. suis to sow infertility. A published PCR method for C. suis was recently validated and implemented at the AHL. Acceptable samples for C. suis PCR include vaginal, rectal, nasal, and ocular swabs, depending on clinical presentation. C. abortus PCR continues to be available at the AHL, and has similar sample requirements.
PCR for Mycoplasma suis, formerly Eperythrozoon suis, is also now available at the AHL. Variably severe hemolytic anemia and associated poor growth caused by M. suis infection may develop in pigs of any age, but especially in nursery and feeder pigs. Infection may also be subclinical. EDTA blood is the preferred sample for M. suis PCR. AHL
OAHN Swine erysipelas project is ongoing
In response to swine practitioners’ identification of increased erysipelas cases in the Ontario herd, the OAHN Swine Network is supporting a project to further investigate and characterize Erysipelas rhusiopathiae isolated from clinical cases and from abattoir samples.
Veterinarians with suspected erysipelas cases are encouraged to contact Dr. Tim Pasma, Ontario Ministry of Agriculture, Food, and Rural Affairs (OMAFRA) to enroll in the project (tim.pasma@ontario.ca).
For enrolled herds, fresh or frozen samples from spleen and lung of affected pigs should be submitted to the AHL for bacterial culture. AHL
AVIAN/FUR/EXOTIC SPECIES
Husbandry and biosecurity of Ontario small poultry flocks
Leonardo Susta, Nancy Brochu, Michele Guerin, Brandon Lillie, Csaba Varga, Marina Brash
The 2-year prospective study about disease surveillance in Ontario small flocks (collaboration between the AHL, OVC, and OMAFRA under the Ontario Animal Health Network framework) was completed in September 2017. The results about pathogen prevalence and causes of morbidity and mortality have been published recently.1,2 The last component of the study included assessment of the demographic characteristics of the participating flocks, through analysis of the results derived from the husbandry and biosecurity questionnaire.
Completing the questionnaire was a requisite for small flock owners to participate in our study, which allowed them to submit their birds for postmortem analysis and microbiological testing to the AHL for a discounted fee. The questionnaire was composed of 41 questions, divided into 2 main subjects: one regarding the flock from which the submitted birds derived (e.g., housing, husbandry, vaccination), and one about the general premises where birds were kept (e.g., presence of bodies of water).
We received 153 valid questionnaires. Most owners (65%) reported chickens as the only poultry raised, 32% raised chickens and at least one other poultry species (i.e., turkeys, waterfowl, gamefowl), and only 2% raised species other than chickens. Most commonly, chickens were kept for egg production (71%), and the most frequently reported reason for keeping birds (answers not mutually exclusive) was personal consumption (69%), keeping birds as pets (38%), and farm gate sales (18%). The majority of owners (75%) had raised birds on their premises for 1 year or more. Owners reported to have acquired birds from many different sources (answers not mutually exclusive), including hatcheries (39%), friends and neighbors (31%), feed stores (16%), and others (49%), such as online advertisements and private breeders.
Only 30% of owners reported to keep birds in an exclusively inside coop or barn; 70% had some type of free-range housing or outdoor access. Overall, owner’s knowledge of effective biosecurity practices was inconsistent or inadequate. For instance, <50% of owners reported to have dedicated shoes or clothing for the coop/barn, <5% reported to use a foot-bath, and >60% reported to allow visitors in the coop/barn, often without biosecurity precautions. Only 37% of owners who sourced birds from hatcheries indicated that birds received vaccination at hatch, while the rest provided a negative answer or were unsure. Only 1 owner reported that birds received additional vaccination on the premises. Based on 61% of questionnaires, some form of medication (e.g., coccidiostat, deworming, antibiotics) had been applied to the flocks in the past 12 mo.
Our results provide baseline characterization of small poultry flocks throughout Ontario, and indicate that management and husbandry practices in these flocks are varied. There are some critical issues, however, that were commonly identified. First, birds are often acquired from non-reputable sources (e.g., private breeders, hatcheries that are not registered through the Ontario Hatchery and Supply Flock Program), increasing the likelihood that birds might be infected at the time of purchase with debilitating pathogens (i.e., Mycoplasma spp.), some of which with zoonotic potential (i.e., Salmonella spp.). Additionally, small flocks hardly ever receive additional vaccinations on farm, underscoring the importance of obtaining birds that are already vaccinated. Although vaccinating small flocks is logistically difficult for even the most well-intentioned owners, purchase of birds from registered hatcheries or co-ops will provide chicks that are protected at least for Marek’s disease virus, or – if ready to lay pullets are sought – for several respiratory pathogens. Marek’s disease and mixed respiratory infections, case in point, were the main causes of death for the birds submitted in our study.2 Lastly, striving for better biosecurity practices will not only decrease the risk of pathogen spread to other flocks (whether commercial or not), but will also reduce the pathogen challenge and avoid precipitating silent respiratory infections, such as mycoplasmosis, if these are already present in small flocks. AHL
References
1. Brochu NM, et al. A two-year prospective study of small poultry flocks in Ontario, Canada, part 1: prevalence of viral and bacterial pathogens. J Vet Diagn Invest 2019;31:327-335.
2. Brochu NM, et al. A two-year prospective study of small poultry flocks in Ontario, Canada, part 2: causes of morbidity and mortality. J Vet Diagn Invest 2019;31:336-342.
New multiplex rtPCR test for 3 psittacine viruses
Daniel Gibson, Nicole Nemeth, Hugues Beaufrère, Csaba Varga, Davor Ojkic, Anna Marom, Leonardo Susta
Psittacine birds (parrots, macaws, etc.) are commonly kept as pets or in private collections. Over the past 20 years, >1,800 psittacine birds have been submitted to the OVC and AHL for postmortem examination, with numerous birds being diagnosed with infection by 3 DNA viruses: aves polyomavirus 1 (AvPyV-1, budgerigar fledgling disease virus), beak-and-feather disease virus (BFDV), and psittacid herpesvirus 1 (PsHV-1). These are important pathogens that can cause significant morbidity and mortality in multiple species of psittacine birds. Until recently, the AHL did not provide molecular tests to detect these viruses, basing the diagnosis mainly on histopathologic evidence and clinical history. Therefore, we developed a multiplex real-time PCR (rtPCR) assay for detection of these 3 viruses and improve the accuracy of diagnosis.
Primers and probes were designed from publically available nucleotide sequences for each virus. In addition to routine analytical validation of the assay, test agreement with histologic diagnoses was performed on archived formalin-fixed, paraffin-embedded (FFPE) tissues from psittacine birds submitted for postmortem examination at the OVC and AHL. To be included in the positive cohort, birds must have showed histologic evidence of infection (i.e., inclusion bodies in tissues). We also included FFPE tissues from presumed virus-negative birds, which showed no signs of viral infection. Results were compared between original histologic diagnoses and rtPCR using percentage agreements to determine in how many cases the tests agreed.
The assay showed high analytical sensitivity, detecting <6 copies of viral DNA per reaction, and 100% specificity as determined by the lack of cross-reactivity with 59 other veterinary infectious agents. Overall, FFPE tissues from 85 psittacine birds were used for diagnostic validation. The multiplex rtPCR assay confirmed 98% of histopathology-positive cases (i.e., those with presence of inclusions), and also identified many subclinical infections that were not detected by histopathology, including coinfections (Fig. 1). Tests showed high overall diagnostic agreement, as confirmed by kappa statistics of 0.71, 0.39, and 0.80 for AvPyV-1, BFDV, and PsHV-1, respectively. Subclinical infections were associated with significantly higher average Ct values compared to cases with histologic evidence of infection for all 3 viruses (Fig. 2), suggesting that subclinical infection is associated with lower viral loads.
Data on the presumed best tissues for testing were opportunistically collected based on the placement of tissues in the paraffin blocks. The most likely samples to return a positive Ct value in infected birds were cassettes including spleen for AvPyV-1, liver or kidney for PsHV-1, and bursa or thymus for BFDV. However, these recommendations will need to be validated by testing single tissues sampled separately at the time of autopsy.
Overall, this new assay has shown good utility to confirm infection by AvPyV-1, BFDV and PsHV-1 in psittacine birds diagnosed by histopathology, as well as to identify silent or latent infections, and will prove to be an effective tool for screening protocols and confirmation of disease also in clinical samples and live birds. AHL

Figure 1. Venn diagram showing the numbers of psittacine birds infected with each virus as determined by a multiplex rtPCR (n = 85). Asterisk indicates one bird that was diagnosed with a APV:BDFV coinfection by histopathology.

Figure 2. Average Ct values of samples from birds with and without viral inclusion bodies in psittacine birds diagnosed with viral infection by rtPCR (n = 61). For each virus, different letters indicate significant differences using 2-tailed t-tests.
HORSES
Atypical cutaneous nodular lymphoid hyperplasia (“pseudolymphoma”) associated with Borrelia burgdorferi infection in a horse
Margaret Stalker, Stefan Keller, Lisa Ledger, Murray Hazlett, Tiffany Richards
Three punch biopsies were received from a 5 x 3 x 1 cm raised mass on the left hindlimb of a 12-y-old Hanoverian mare, located near the base of the hamstrings (Fig. 1). On histologic examination, the biopsies revealed nodular-to-diffuse dermal infiltrates of lymphocytes forming discrete follicular structures, often with prominent germinal centers and eccentrically positioned peripheral mantle zones of smaller mature lymphocytes (Fig. 2). The presumptive histologic diagnosis was atypical cutaneous nodular lymphoid hyperplasia. Additional clonality testing targeting the equine B lymphocyte immunoglobulin heavy chain locus (IGH) revealed polyclonal rearrangements with 2 different primer sets (FR2/FR3), supporting the diagnosis of a reactive rather than a neoplastic process. Interestingly, this was the second such biopsy we have received from 2 unrelated horses from this practice over the last 2 years.
A literature search of this unusual cutaneous lesion revealed two published reports, the first a single case report from a horse with multiple dermal papules developing at the site of previous removal of an engorged tick.1 This horse subsequently tested positive by serum ELISA and western blot for Borrelia burgdorferi, and a PCR assay using primers targeting the B. burgdorferi ospA gene, run on formalin-fixed paraffin-embedded (FFPE) tissue, was also positive. The lesions in this horse resolved following a 30-day course of doxycycline therapy.
The second was a conference abstract reporting 19 cases of so-called “pseudolymphoma”, a term borrowed from the human literature to describe this non-neoplastic lymphoproliferative process.2 One of the 19 cases was also positive for B. burgdorferi, again using PCR primers targeting the ospA gene. Based on these reports, we ran a screening qPCR assay for Borrelia spp. on the FFPE from both of the AHL equine biopsy cases, targeting a 75-bp fragment of the 23S rRNA region of B. burgdorferi. Both cases were positive for Borrelia spp., however only the recent case was confirmed positive on the second-step confirmatory qPCR test targeting the B. burgdorferi OspA gene. Subsequent serologic testing of the mare was also positive on the equine Lyme disease multiplex assay.
In humans, development of cutaneous pseudolymphoma has been associated with various localized antigenic stimuli, including injected irritants/foreign substances such as drugs, vaccines or tattoo ink, arthropod bites, and infectious agents including B. burgdorferi, although most cases remain idiopathic. The veterinary practice submitting these 2 equine cases is located in an area of eastern Ontario experiencing a significant expansion of tick populations, including Ixodes scapularis, the vector of Lyme disease, and several ticks were anecdotally removed from the mare over the course of the preceding autumn. This case highlights an unusual manifestation of an emerging disease in Ontario. AHL
References:
1. Sears KP, et al. A case of Borrelia-associated cutaneous pseudolymphoma in a horse. Vet Dermatol 2012;23:153-156.
2. Malatos JM, et al. Histologic and immunohistochemical characteristics of 19 cases of equine cutaneous pseudolymphoma and the association with Borrelia burgdorferi. Proc Am College Vet Pathol Ann Mtg, Vancouver, BC, Nov, 2017.

Figure 1. Skin lesion, left hind leg.

Figure 2. Histology of skin lesion.
COMPANION ANIMALS
Common causes of puppy mortality diagnosed at the AHL, 2015-2018
Margaret Stalker, Maureen Anderson
As part of the OAHN Companion Animal disease surveillance network, we investigated causes of mortality in puppies submitted to the AHL for postmortem examination from Sept 2015 to Dec 2018 (n = 75). Cases were subcategorized by age (birth to 2 wks, 3-8 wks, 9-16 wks). Clinical signs were often similar regardless of age or etiology, including listlessness, fading or dying pups, or pups found dead. Some exhibited diarrhea and/or vomiting prior to death.
In all age groups, bacterial etiologies were the most frequent infectious diagnosis (Fig. 1), and included bacterial/aspiration pneumonia and/or septicemia (Streptococcus canis, Staphylococcus pseudintermedius, Escherichia coli, Pasteurella canis, Klebsiella spp., Streptococcus lutetiensis, Enterococcus faecalis, and Histophilus haemoglobinophilus were the dominant bacterial isolates), and diarrhea/enteritis (attaching, attaching/effacing, enteropathogenic, and hemorrhagic strains of E. coli, and Campylobacter jejuni).
Viral diseases included canine herpesvirus, canine parvovirus (including parvoviral enteritis and parvoviral myocarditis), and canine coronavirus.
Protozoal diseases included systemic neosporosis and coccidiosis.
Congenital anomalies included cleft palate, small intestinal stenosis, pectus excavatum, ectopic ureters with cystitis/pyelonephritis, atrial septal defect, hepatic biliary aplasia, and nephropathy.
Lesions in the category of trauma included mismothering, and included emaciation/dehydration, diaphragmatic rupture/herniation, and thermal burns.
Miscellaneous conditions included mesenteric volvulus, gastric foreign bodies, and peracutely aspirated food. AHL

Figure 1. Common causes of puppy mortality diagnosed at the AHL, 2015-2018.
African swine fever alert for companion animal/mixed practitioners:
Please see “African swine fever – resources for veterinarians” on page 22 of this Newsletter.
Entry of ASF into North America would be devastating to our swine industries as a result of border closures and lost trade. Border controls have been tightened (and more sniffer dog teams) to prevent inadvertent entry of foodstuffs in travellers luggage. Feed suppliers are well aware of the threat of importing ASFV in feed ingredients.
ASF virus easily persists and can be transported in cured meats. Should these slip through security and be shared with pet pigs, ASF could appear in our backyard. Please be alert to unexpected illness in pet pigs!