U of G research sheds new light on origins of bipolar disorder

A new study by researchers from University of Guelph’s Department of Molecular and Cellular Biology provides a new perspective on bipolar disorder, a poorly understood and under-researched mental health disorder affecting about 1-2 per cent of Canadians, or about 400,000 people. The study, published in the journal Molecular Psychiatry, provides strong evidence that the disorder is neurodevelopmental in origin.
Bipolar disorder, previously known as manic depression, is characterized by fluctuating episodes of extreme emotional highs (mania) and lows (depression). The disorder is highly heritable, but the role of environmental factors is less clear. Because of the poor understanding of the origin of the disorder, treatment options have been limited to managing patients’ symptoms, often with a mood stabilizer known as lithium.
Since bipolar symptoms most often appear in late adolescence or early adulthood, past research has focused on studying mature or post-mortem brain cells from donors, but this approach missed changes very early in the brain’s formation.
For this study, U of G researchers from Dr. Jasmin Lalonde’s lab started earlier, analyzing differences in neural progenitor cells, which are early-stage cells that can differentiate themselves into many other types of neural cells. Researchers cultured stem cells from patients with bipolar disorder and compared them to cultured stem cells from healthy individuals.

“Our study looks at bipolar disorder through a new lens,” says co-lead author Dr. Tristen Hewitt, who completed the research as part of his PhD at the U of G and is now a postdoctoral fellow at the University of Helsinki in Finland. “From this lens, we can look at alternative ways to study the disease. That will eventually lead to the treatment.”
Differences start at the molecular level
Researchers started at the molecular level, examining a system called store-operated calcium entry, which transports calcium into neurons to control processes important for growth and activity. They found that this system was dysfunctional in the neural progenitor cells derived from donors with bipolar disorder, compared to those from healthy individuals.
Since calcium plays an important role in gene expression, they then sequenced the genes of these “immature” neurons. They found hundreds of genes that were expressed differently than those from healthy individuals, with many of those genes involved in neurodevelopment.
They then took a step back to examine the function and behaviour of neural progenitor cells, finding that these neurons replicate slower, but migrate more and have longer neurites – the connections between neurons – than those from healthy individuals.
Creating mini brain-like organs
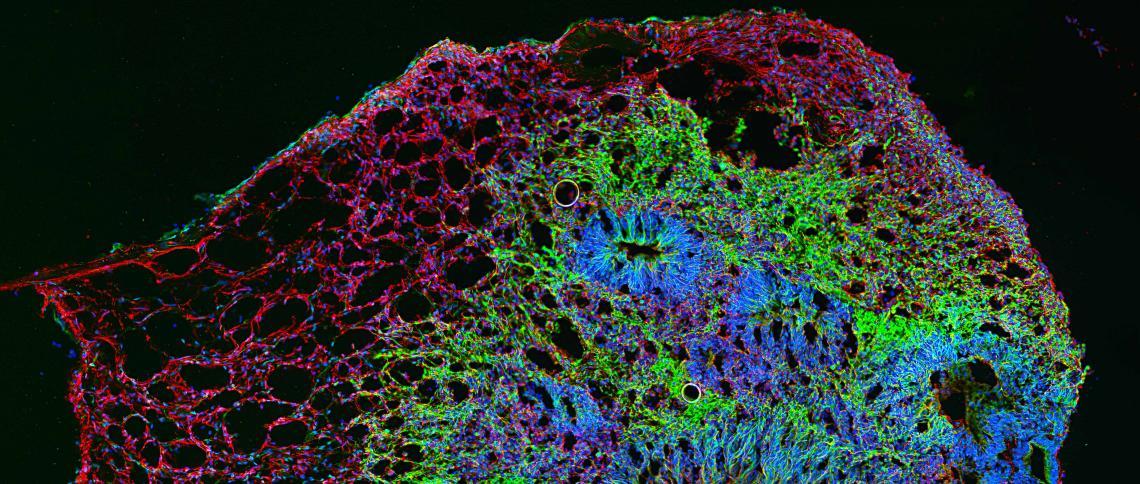
Since studying brain cells in a dish can’t show researchers how these neurons might organize themselves should they be allowed to grow in three dimensions, researchers turned to a newer research tool. Using stem cells from both bipolar and healthy individuals, they cultured mini three-dimensional (3D) brain-like organs called cerebral organoids.
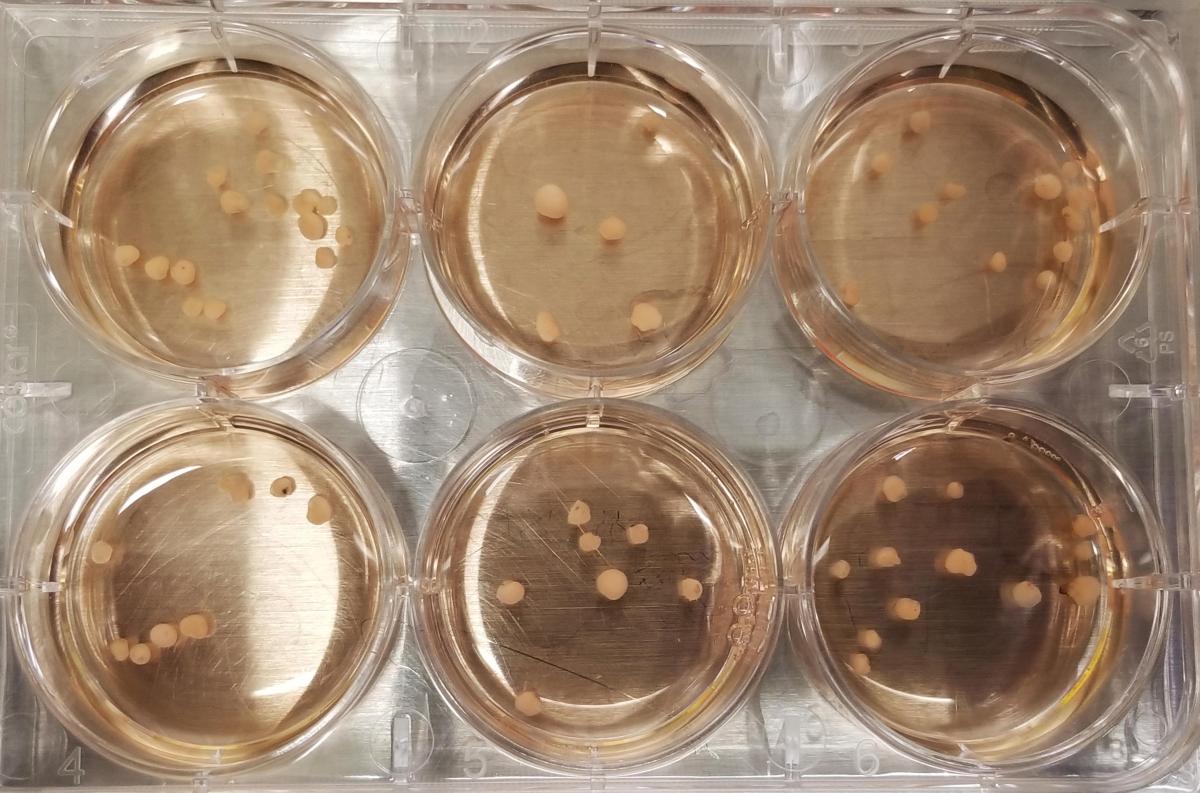
“If you grow neurons on culture dishes, they won’t make the same 3D connections they make in the brain,” says co-lead author Dr. Begüm Alural, a postdoctoral fellow in MCB. “With the cerebral organoids, the neurons develop as they connect with each other. It’s really groundbreaking because it lifts our research from a single layer into actual 3D brain tissue.”
Thanks to the organoids, which mimic the early stages of brain development, researchers were able to see that the areas on the organoid where immature neurons differentiate and migrate were smaller and thinner than those made using stem cells from healthy individuals.

Diagnoses may be possible earlier
The results of the study have significant implications for future research on the origin and treatment of bipolar disorder, but the findings also lend weight to a growing body of evidence that it may be possible to diagnose the disorder at a younger age, rather than just at the onset of symptoms in late adolescence or early adulthood.
Future research in Dr. Lalonde’s lab will examine whether it’s possible to induce bipolar disorder in animals by transplanting immature neurons. If they’re successful, animal models could someday be used to better study the disorder, including potential treatment options.
The study was completed over seven years, with support from researchers across the university, including PhD, master’s and undergraduate students, a postdoctoral fellow, Dr. Lalonde and Dr. Nina Jones from MCB and Dr. Melissa Perreault from the Ontario Veterinary College. The stem cells for the study were derived from a biobank at Massachusetts General Hospital in Boston, with support from Dr. Roy Perlis, founder and director of the Center for Quantitative Health. Funding for the study was provided by the Brain and Behavior Research Foundation, the Canadian Foundation for Innovation and the U of G.