Race Against Resistance: Protein Profiles Reveal New Potential Target for Antibiotics
The medical progress of the last century is in peril. The threat? The rise of bacteria that are resistant to antibiotics.
“Cancer therapy, surgeries, maternal health — all the medical advances since the 1940s are predicated on the use of antibiotics,” says Dr. Cezar Khursigara, a researcher in Molecular and Cellular Biology whose work on antibiotic resistance was recently published in the journal mSystems.
The threat is particularly acute for people with cystic fibrosis, a genetic disease in which mucus accumulates in the lungs, providing the ideal breeding grounds for harmful bacteria to proliferate.
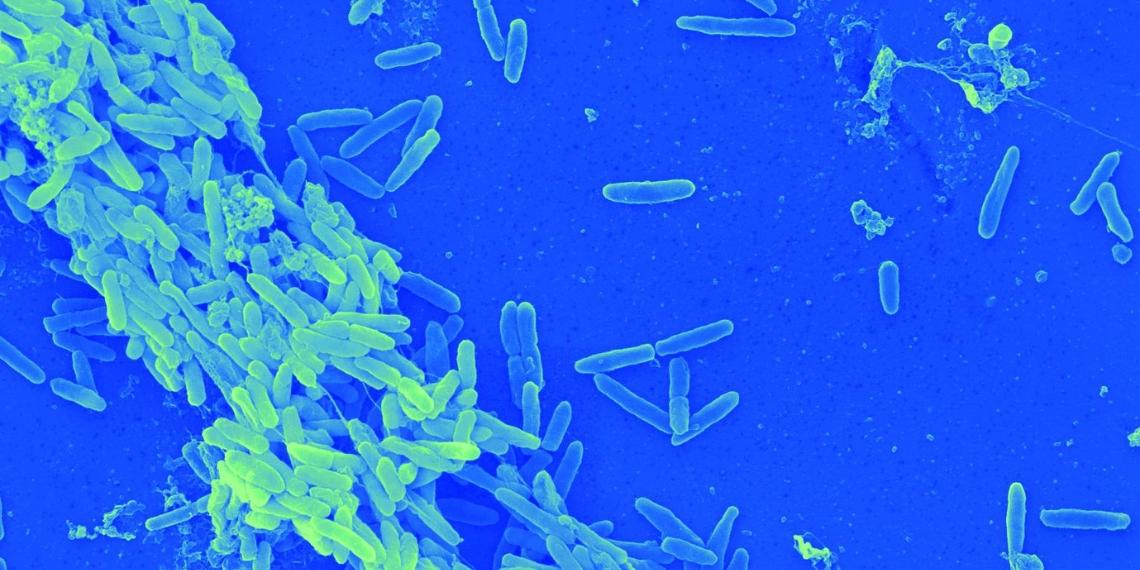
“People with cystic fibrosis have a defective membrane protein that affects the movement of solutes in and out of cells,” explains Khursigara. “By the time they reach their early twenties, Pseudomonas aeruginosa becomes the dominant pathogen in their lungs and remains so for the rest of their lives.”
Pseudomonas infections — whether in the lung or elsewhere — are often treated with beta-lactam antibiotics, a class of crucial first-line antibiotics related to penicillin. They work by weakening the cell walls of bacteria to the point where it is no longer viable.
However, most research into antibiotic resistance relies on laboratory strains of P. aeruginosa, which do not behave the same way as those found in people with infections. Khursigara’s group honed in on these differences by comparing a common laboratory strain of P. aeruginosa with strains isolated from patients.
“The clinical lines we used are epidemic strains that are a significant issue in cystic fibrosis clinics. While work on classical laboratory strains is valuable, it’s also important to look at a diversity of strains to get a better understanding of their impact in a clinical setting,” says Khursigara.
Bacteria’s short generation times — within 24 hours, a single Pseudomonas cell can multiply to almost a billion cells — means that mutations that allow a cell to survive an antibiotic onslaught can quickly become widespread. This leads to the reliance on, and inevitably resistance to, increasingly more advanced antibiotics.
One strategy to understand how exactly P. aeruginosa evolves resistance is to use proteomics, where researchers identify the proteins produced by the bacteria upon exposure to antibiotics.
“We generated a snapshot of all the different proteins and their relative abundances,” explains Khursigara. “Essentially, proteomics tells us what the cell is doing differently when it is exposed to antibiotic pressure.”
Under antibiotic treatment, all strains exhibited a well-known response, wherein they increased their production of proteins involved in pumping out antibiotics.
“Pseudomonas has efflux pumps that get activated by antibiotics and actively secrete them,” explains Khursigara. “The more antibiotic comes in, the more they pump out.”
However, the researchers also found that laboratory and clinical strains had distinct protein profiles that were unrelated to the activation of the efflux pumps.
“One of the clinical strains overproduced a suite of proteins related to keeping the cell intact and helping it divide effectively,” says Khursigara. “Essentially, these cells were able to maintain their integrity by brute force despite the antibiotic. This is a resistance mechanism that has yet to be well studied.”
This unexpected finding further highlights the importance of using clinical isolates in research.
“The mechanism underlying the resistance in our study would not be on our target list for the development of new antibiotics if we had only used non-clinical isolates,” Khursigara points out. “However, if we look at antibiotic resistance from as many different angles as possible, we can get some clues as to how to combat it.”
How exactly this particular resistance mechanism functions is still a mystery — one which Khursigara’s group is already working to solve. Indeed, as our arsenal of effective antibiotics continues to dwindle, identifying potential new targets for antibiotics becomes even more crucial.
Ultimately, Khursigara hopes that this work will help develop new antibiotics and, eventually, feed back into clinical settings and improve outcomes for patients. In the race against the rise of antibiotic resistance, such work is critical if we are to avoid returning to a pre-antibiotic world.
This study was funded by the Canadian Institutes of Health Research.
Read the full study in the journal mSystems.
Read about other CBS Research Highlights.